In the realm of healthcare governance, the ongoing saga between the government and medical professionals reveals a disturbing pattern: superficial attempts at resolution that ultimately mask the deeper structural failures of our health system. The recent negotiations between the Health Secretary and the British Medical Association (BMA) underscore this dissonance. While official narratives celebrate diplomatic efforts, the underlying issues of underfunding, undervaluation, and systemic neglect persist and deepen. It is naive to believe that these political maneuvers—allowing local trust leaders to make decisions or offering superficial pay raises—are sufficient to address the fundamental challenges confronting the NHS.
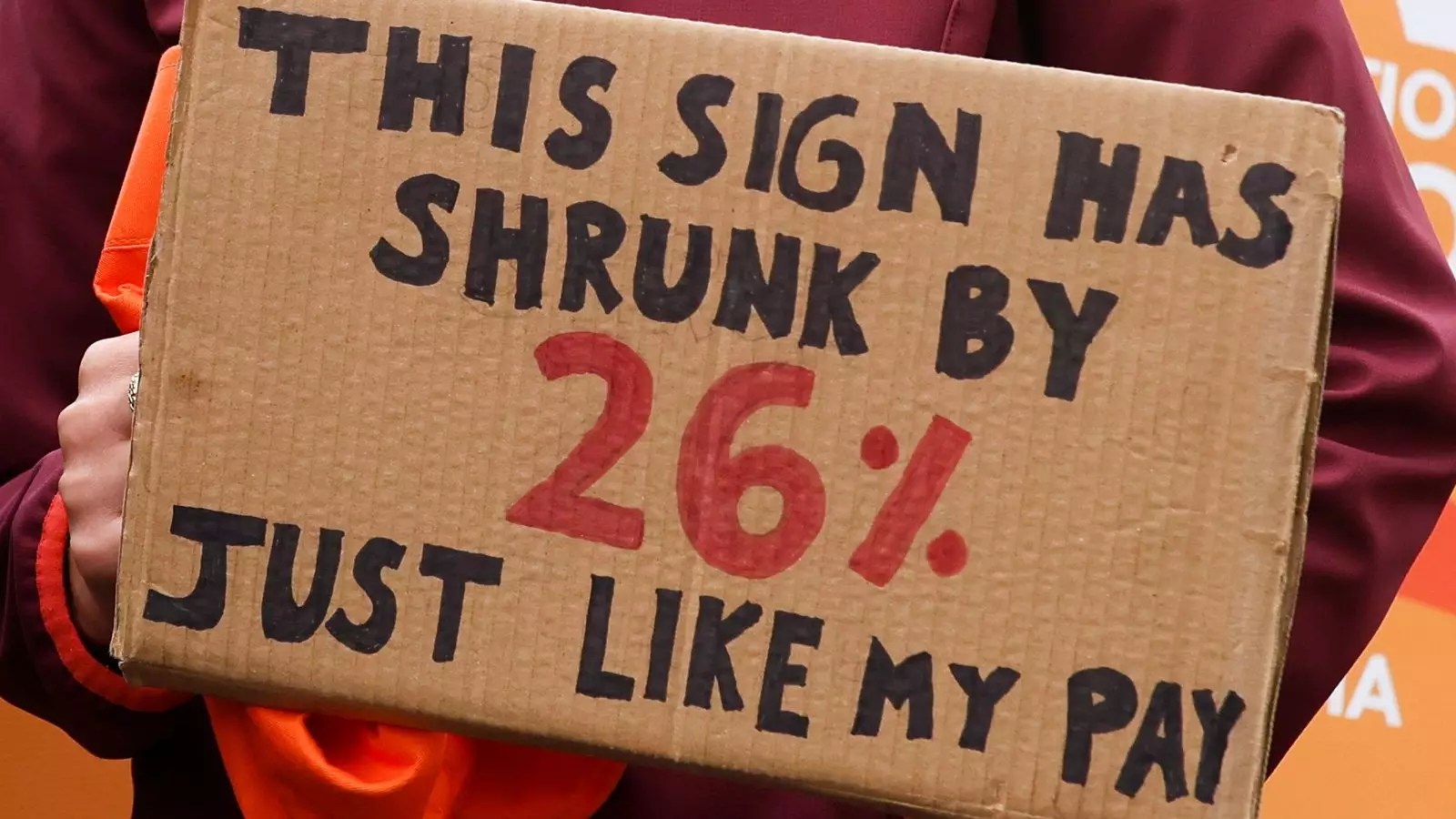
The government’s rhetoric paints a picture of progress—a 29% pay rise in recent years, a supposed testament to their efforts to retain medical staff. Yet this portrayal ignores the reality faced by resident doctors: years of stagnation in real terms, with many earning roughly £18 an hour, and demands for a modest increase to £22. This gap, framed as “reasonable,” conceals the fact that the core issue isn’t just about numbers. It is about respect, recognition, and the acknowledgment of a workforce that has been undervalued for nearly two decades. Treating pay as a negligible factor perpetuates a narrative that our medical professionals are somehow overpaid, ignoring the essential role they play in upholding a functioning health system.
A Distraction from Systemic Flaws
The superficial solutions proposed—like granting local authorities autonomy—are symptomatic of a government desperate to avoid confronting the broader failures of NHS funding and leadership. While decentralizing decision-making might offer short-term flexibility, it fails to address the core issue of resource scarcity and systemic underinvestment. This approach is a classic tactic: shifting blame and responsibility downstream, away from the policymakers who have perpetuated underfunding and neglect. The real question remains: does relying on local discretion genuinely protect patients or merely mask the scale of the crisis? Historically, such decentralization has led to patchwork solutions that crumble under pressure, especially when crucial staffing levels are compromised.
Furthermore, the narrative of “urgent” and “non-critical” care becomes a bureaucratic game rather than a patient-oriented strategy. Labeling certain cases as urgent merely shifts the discretion of risk onto overstretched staff, many of whom are working under unsafe conditions due to staffing shortages and burnout. This approach may temporarily reduce visible disruptions, but it ignores how systemic underfunding creates an environment where patient safety is compromised not from malicious intent but from institutional failure.
The Real Cost of Underinvestment and Political Posturing
The core problem lies in the chronic underfunding of the NHS, which has been ongoing for nearly two decades. Governments—regardless of political color—have prioritized short-term political gains over long-term investment in healthcare infrastructure, workforce development, and technology. The costly illusion of pay raises and local decision-making distracts from the fact that without adequate funding, hospitals cannot retain staff, nor can they provide the quality of care that patients deserve.
The discourse around pay raises, strike threats, and political blame-dividing undermines the fundamental goal of a humane, equitable healthcare system. This is not merely a labor dispute but a symptom of a deeper malaise—an institutional failure to prioritize healthcare as a national necessity rather than a political bargaining chip. The public’s waning support for strikes reflects societal fatigue with ongoing crises that are permitted to fester because of political incapacity or unwillingness to confront the truth: we have starved a vital system of resources for far too long.
In this larger picture, the negotiations are less about resolving immediate disputes and more about whether the political will exists to finally confront the inconvenient truth—that meaningful reform requires genuine investment and a willingness to challenge entrenched interests. As long as decisions are made based on optics rather than needs, the NHS’s crisis will deepen, and the trust in both political leadership and professional integrity will continue to erode.